About the Nossal Institute
Our purpose
Nossal Institute's purpose is to improve the health of all people globally by deepening our collective understanding of how multiple systems operate and interact to shape health through applied research, learning and partnership.
Our goal
We aim to support the strengthening of health systems towards achieving health equity, inclusion, sustainability, people centredness, resilience and security.
We are systems thinkers
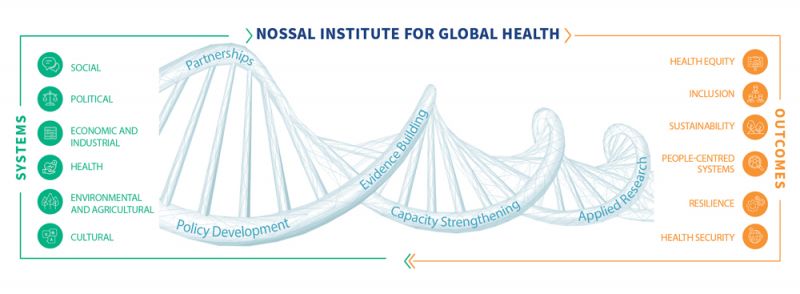
Achieving health and wellbeing for all, necessitates recognising health outcomes are reliant on multiple relationships, processes and systems. Complex interaction between political, social, cultural, economic (including industrial), agricultural and ecological factors influences our health system and our health. Using a systems lens, the Nossal Institute for Global Health’s multi-disciplinary team of experts work with partners to formulate, explore, monitor and evaluate policies, strategies and programs in different settings for their impact on the health and wellbeing of people drawing on and contributing to an evidence based understanding of how these systems interact.
Ultimately, we use systems thinking to advance health equity, inclusion and sustainability.
Partnerships are at the heart of our work. We work with governments, academics, philanthropists, multilateral agencies and civil society partners to influence health outcomes for all through evidence building and applied research. We share and translate our research into policy and practice, as well as education, learning and capacity strengthening for current and future leaders.
How do we apply systems thinking?
We seek to understand the operation of systems in the real world. We focus on the contexts in which they were designed and operate, explore both their intended and unintended consequences and consider how they can equitably and best serve the health of populations
We draw on our trusted and extensive partnerships in the Asia Pacific and beyond to undertake collaborative research, engaging our collective expertise across a broad range of disciplines.
We communicate and translate knowledge into policy and practice. Our teaching and learning experts integrate these insights and learnings from our research into degree programs, short courses, and continuing professional development programs.
Our approaches
We support evidence building, capacity strengthening, applied research and evaluations, policy development and work in partnerships.
-
Evidence building
We explore different elements of systems to build understanding of how social, political, economic, health, agricultural and cultural systems operate and interact to impact health at the global, national and local levels.
-
Capacity strengthening
We work with partners to develop relevant and sustainable skills, structures and resources across the partnership.
-
Applied research
Our researchers are at the leading edge of discovery to develop, test and validate approaches to improving global health.
-
Policy development
We use our expertise to work with decision makers to develop and improve policies that promote the health well being of communities and support their implementation.
-
Partnerships
Partnership is essential to everything we do. It ensures relevance, quality, sustainability and ownership.
Our work
We establish and extend the evidence base for strengthening health systems and extending universal health coverage to ensure access to health care and to promote well-being across our region’s diverse communities.
The Nossal Institute is multi-disciplinary. We draw on academic and professional expertise from a broad range of disciplines, sectors and regions for our applied research, teaching and leadership.
Disability, Inclusion and Rehabilitation
We support equitable development through the design and delivery of tools, strategies, research and training to overcome discrimination and ensure the participation of the most disadvantaged population.
Our work delivers practical targeted and mainstreamed solutions for real world impact. Meet our team & see our projects
Education and Learning
We take a holistic approach to education, combining academic excellence with real-world relevance. Systems-thinking, creative problem-solving and interdisciplinary collaboration are at the heart of all our work. Find out more
Health Systems Governance and Financing
We support countries to improve equity in access to and utilisation of quality health services, while responding to changing health needs. We undertake applied research to inform, monitor and evaluate health system strategies, programmes and interventions.
We aim to strengthen the foundations of health systems – their governance, funding arrangements and policy frameworks – to better support the delivery of effective services and programs. Meet our team & see our projects
Social & Cultural Dimensions of Health Systems
We use theoretical and methodological insights from across the social and health sciences to support countries to better understand and transform their health systems to effectively deliver good quality and responsive services, equitably. In all our engagements we take a people-centred approach, and have an explicit focus on partnerships, learning, and strengthening of capacities across communities and health systems. Meet our team & see our projects
One Health
One Health research combines the elements of environmental-health, animal-health and human-health for a common goal. It considers the interdependent needs of different populations and sectors of the economy in securing human, animal and environmental wellbeing, and how this is addressed by governance, decision-making structures and processes, communication, and actions across institutions and communities. Meet our team & see our projects
Emerging Programs in Global Health
The Emerging Program team are multi-disciplinary applied researchers responding to emerging priorities in Global Health. Our team members have disciplinary expertise in demography, economics, engineering, psychology, and statistics, and are engaged in delivering evidence-based research and training to support the work of Australian and international stakeholders across a wide range of areas of public health relevance, including measurement and data analysis, mathematical modelling, law enforcement, well-being and livelihoods, gender and living spaces, urban resilience, and programmatic and economic evaluations. Meet our team & see our projects
Gender and Women’s Health
We aim to advance the health of women in Australia and internationally, to reduce inequity and create positive change. We are building evidence about systemic and service-based opportunities to promote positive health and wellbeing for children, families and communities. Through research, teaching and public engagement, our work contributes to a robust knowledge base about the health effects of gender inequity and its intersection with social, economic and cultural factors. Meet our team & see our projects