Economy and public health: Partners or rivals?
Health and economy are generally viewed as mutually supportive. Health relies on an economy that can offer the population sustainable livelihoods that support good nutrition, safe water and sanitation, weather protected shelter and other basic needs. Evidence suggests, in the long run health improves as economic capacity grows beyond that essential level and as health expenditure increases at higher levels, the economy improves. The economy relies on a heathly workforce that fulfils its potential in terms of both physical and mental capacities. Malnutrition in childhood, for example, affects education attainment and in turn the opportunity to contribute to a skilled workforce.
At the outset of the COVID-19 pandemic, it seemed that health and economy had suddenly become rivals, or even deadly foes. Many, not only those on the populist right, argued that we had to choose between business closures, unemployment, poverty on the one hand and deaths, disease and chronic ill health on the other. Countries made drastically differing choices about whether or not to suspend a level of economic activity with “stay at home” orders to prevent the spread of the virus. Others toyed with the idea of ‘herd immunity’ hoping to emerge with a virus-resistant population and economy back to full operation, at the fastest speed, albeit recognising that the cost would be a significant death toll, especially among the elderly.
Things look pretty different in mid-2021. What has been the economic trajectory of those countries that apparently chose public health, and accepted restrictions on economic activity such as lock downs and border closures to control the virus, and those that chose to keep their economies as open as possible at the expense of increased virus transmission?
We’ve graphed the major macro-economic outcomes: GDP growth and unemployment, for the seven countries that have so far experienced at least 100,000 deaths and a death rate per 10,000 population of at least 100 (sourced from the Hopkins COVID-19 data site) and seven countries that have reported death rates of less than around 5 per 10,000 population (we’ve included Thailand with a rate reported today of 5.06).
These are not the only seven that meet the low death rate criterion. Most of the others that do are in Africa, and we need to be aware of two issues. First, they seem collectively to have dodged COVID-19 in 2020 without there being a clear explanation related to economic restriction. Second, data reliability is often poor. It will be more important to put the African experience into context after 2021, as the Delta variant is now posing similar questions in Africa as were posed in the rest of the world last year. The other countries we’ve excluded from consideration are Brunei (too small) and Laos, Cambodia, Papua New Guinea and Uzbekistan (on the grounds that the IMF database does not provide unemployment data).
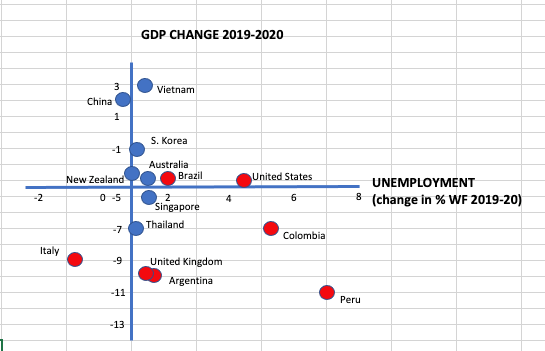 We’ve graphed the two sets of countries against GDP growth and change in unemployment level (as a % of the workforce) between 2019 and 2020, using IMF data. The apparent conclusion is that low COVID death rate countries (blue) effectively implemented public health programs to limit COVID infections and succeeded in supporting economic activity in the presence of restrictions. Countries with high COVID death rates (red) are those which largely ignored or bungled the public health measures with a vain hope of avoiding economic cost. Peru, with the biggest increase in unemployment and the biggest loss of GDP, has so far suffered the highest COVID death rate per head of population in the world. China and Vietnam, with the highest GDP growth and in China’s case, a reduction in unemployment, have also reported the lowest and second lowest COVID death rates.
We’ve graphed the two sets of countries against GDP growth and change in unemployment level (as a % of the workforce) between 2019 and 2020, using IMF data. The apparent conclusion is that low COVID death rate countries (blue) effectively implemented public health programs to limit COVID infections and succeeded in supporting economic activity in the presence of restrictions. Countries with high COVID death rates (red) are those which largely ignored or bungled the public health measures with a vain hope of avoiding economic cost. Peru, with the biggest increase in unemployment and the biggest loss of GDP, has so far suffered the highest COVID death rate per head of population in the world. China and Vietnam, with the highest GDP growth and in China’s case, a reduction in unemployment, have also reported the lowest and second lowest COVID death rates.
Of course, there are caveats to this interpretation. We’ve controlled for no extraneous factors, and it might well be noted that the red countries are largely in the Americas, with a couple in Europe, while the blue countries are largely in South East Asia, with a couple in Australasia. There are likely to be other differentiating characteristics in factors affecting economic performance. The UK’s outlying GDP reduction, only Peru and Argentina do worse in this respect, might also have been influenced by its withdrawal from the European Union.
It’s hard not to conclude that short term economic restriction has paid off for the blue countries in the long term in both reduced death rates AND better economic outcomes. This offers clear policy advice for ongoing pandemic management as countries progress towards adequate vaccine coverage. Even so, not all countries are in the same position economically and socially. The dramatic continuing vaccine shortages as new waves of the pandemic hit across Africa and some low and middle income countries, including Indonesia, provides an additional challenge. Lockdowns, as practised in Australia and New Zealand, are clearly not feasible where a large share of the population relies on daily earnings to finance basic needs.
When the state cannot offer subsidies to compensate for lost earnings, both lacking fiscal space and the administrative systems to do so, and where housing arrangements are crowded and fail to consistently separate households there are significant public health and economic consequences. This lesson was learnt painfully in India. Looking to the experiences of Vietnam, Thailand and perhaps China may offer the most relevant guidance for these countries as they confront the pandemic.
This article was written by Professors Barbara McPake and Peter Annear.
Sign up to Issues in Global Health to receive regular thought pieces on current issues in Global Health delivered to your inbox.
More Information
Professor Barbara McPake, Director, Nossal Institute for Global Health