Implementation Science to Improve Global Health
Resource Platform for Knowledge and Practice
WHO Collaborating Centre on Implementation Research for the Prevention and Control of Noncommunicable Diseases
This website provides resources and supports for implementation research for researchers, program implementers, public health professionals and policy-makers, globally.


In this guide we provide an introduction to basic implementation research terms and concepts and briefly outline what implementation research involves. We have collated and summarized recent relevant evidence and provide links to resources for further information on many of the topics covered. The guide also includes case studies that showcase examples of the implementation of NCD prevention and control policies and interventions. At the end of the guide we provide some practical tools to support the implementation research process.

Purpose and objectives of this website
Although some practical tools for facilitating the use of implementation research for the prevention and control of disease already exist, these mainly focus on communicable diseases. None exist specifically for NCDs. The main purpose of this guide is to provide practical guidance, tools and examples for implementation research so as to support effective implementation of NCD policy options and cost-effective interventions. Specific objectives of this guide are to:
- raise awareness about the purpose and potential impact of implementation research;
- assist countries to capture, collate and analyse information and to translate and adapt evidence-based policy options and interventions to local contexts;
- help identify barriers to the implementation of policies and interventions;
- help identify the best approaches to implementation research.
What is implementation research?
Implementation research investigates the various factors that affect how a new policy or intervention may be used (or implemented) in real-life settings. Such research remains relatively new to population-based health programmes, so a common language and terminology are still being developed. For reference, key terms used in this guide are outlined below.
Questions addressed by implementation research include:
- Which policy or intervention is best for a new context?
- What is the best way to implement it?
- How can the target population be reached?
- What factors might affect implementation and adoption?
- How can the costs of implementation be minimized?
- How can uptake and health outcomes be improved?

-
Implementation
A specified set of activities designed to put into practice a policy or intervention of known dimensions.(15)
Implementation processes are:
- purposeful
- described in sufficient detail to allow independent observers to detect the presence and quality of the specific set of implementations-related activities(16)
-
Implementation research
The scientific study of the processes used to implement policies and interventions and the contextual factors that affect these processes.(17)
Investigates all aspects of implementation, including:
- the uptake of evidence-based policies and interventions
- activities used to put these into practice
- factors that influence these activities
- impact of factors on health outcomes
-
Implementer(s)
An individual (or group of individuals) responsible for management of the implementation process.
Some examples:
- policymakers
- health professionals
- community-based organizations
-
Consumers
The group(s) of individuals that are targeted by an intervention, programme or a policy.
Typically, they:
- are at high risk of developing NCDs, or
- have a high prevalence of NCDs
-
Context
The setting within which a policy or intervention is to be implemented.
Includes all characteristics of said setting, for example:
- stakeholders
- social, economic and political environment
- geographical setting
- epidemiologic profile
-
Knowledge synthesis
The identification, assessment and collation of evidence.
This process:
- relates to existing policies and interventions
- aims to achieve a desired outcome
-
Knowledge exchange
The process of collaborative problem-solving.
This occurs throughout the implementation process between:
- researchers
- decision-makers (including policymakers)
- consumers
- other relevant stakeholders
-
Knowledge translation
The process by which relevant research information is made accessible and available.
Through interactive engagement with audiences, this is used for:
- practice
- planning
- policy making

Why is implementation research important?
One of the purposes of implementation research is to support the successful selection of policies and interventions that have been shown to be efficacious.(16) It also helps identify how to implement these policies and interventions in contexts where populations and/or resources may differ from that where they were initially formulated and evaluated and helps identify which components of a policy or intervention are needed to obtain intended outcomes. Moreover, when prevention and control efforts fail, implementation research can help identify whether failure was due to a policy/intervention being ineffective in the setting (intervention failure) or whether a so-called good policy/intervention was deployed incorrectly (implementation failure).(18)
In effect, implementation research is about learning how to optimize implementation, scale up promising strategies, evaluate impact and, importantly, how to sustain these strategies over the long term. Notably, implementation research has the potential to bridge the evidence-into-action gap.
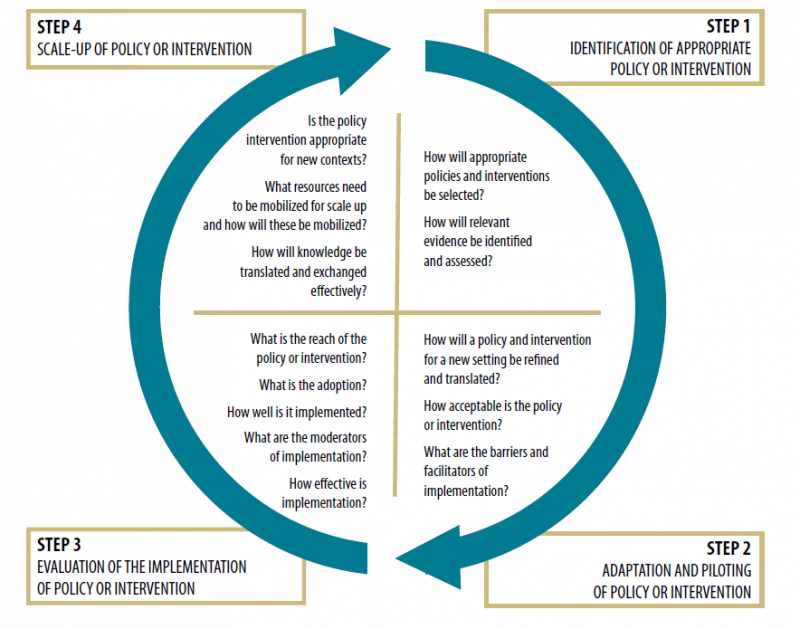
Implementation and the implementation research cycle
There is a growing number of theories and models describing implementation and the implementation research process.(19-22) Implementation typically involves a step-wise, cyclical process (Fig. 1).
The first step is to work with key stakeholders in order to define the specific health need and then identify an appropriate policy or intervention to address that need. The second step is adaptation of the selected policy or intervention to the local context and undertaking some piloting. The third step involves implementation of the adapted policy or intervention. The fourth and final step is assessing if the adapted policy or intervention can be more widely implemented or scaled up and, if so, defining the resources and further steps that will be required to achieve this.(23, 24)
In practice, the path from selection (step 1) through to scale up (step 4) is rarely direct, as it is usually determined by multiple stakeholders, the availability of resources and other contextual factors. Instead, it normally has numerous iterations involving going back and forth between two or more process steps.
This cyclical process is often depicted in implementation models and frameworks. One commonly used framework is the Knowledge to Action Cycle outlined by Graham et al.(25) The KT Clearinghouse provides a range of resources, tools and information about this model.
The burden of noncommunicable disease
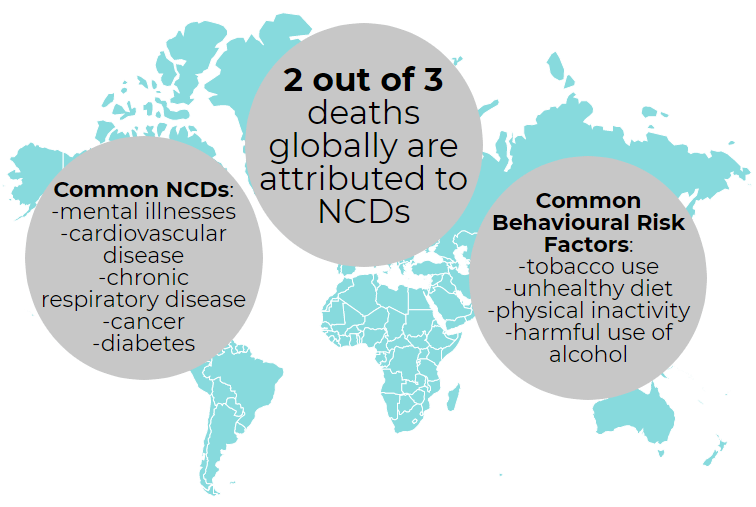
Noncommunicable diseases (NCDs) are noninfectious health conditions typically caused by genetic and/or environmental and lifestyle factors.
As NCDs tend to be long-lasting or recurrent, they are sometimes also referred to as chronic diseases.(1)
Currently, NCDs account for almost two-thirds of deaths globally.(2)
Global response to NCDs
In 2011, the World Health Organization (WHO) published A prioritized research agenda for the prevention and control of noncommunicable diseases,(3) which identified key areas of research relating to the prevention and control of NCDs. In September of that year, participants at the United Nations High-level Meeting on Noncommunicable Disease Prevention and Control recognized the existence of cost-effective interventions regarding the preventability of NCDs and the numerous opportunities for global action, and subsequently The Sixty-sixth World Health Assembly endorsed the Global Action Plan for the prevention and control of noncommunicable diseases 2013–2020.(4) This called upon international partners to take coordinated action to attain nine voluntary global NCD targets by 2025 – including a 25% reduction in premature mortality due to NCDs.
One of the Global action plan’s main objectives focuses on research. This objective calls on stakeholders to promote and support:
- national capacity for high-quality research related to the prevention and control of NCDs (and so, increase the knowledge base for national, regional and global action);
- the translation of high-quality NCD basic research into practice;
- development for the prevention and control of NCDs.

Achieving national goals and targets in relation to NCDs: The evidence-implementation gap
A major challenge in the prevention and control of NCDs has been that despite a wide range of global, regional and national plans, initiatives, policies and interventions, the impact on health outcomes still needs to be increased significantly. There is still a very notable ‘evidence-into-implementation (or action)’ gap. This translation gap – between research evidence and practice – is now very well recognized in many health fields.(5-7)
For example, a review of healthcare delivered to adults from the USA shows that up to 45% of patients fail to receive treatments that have been shown to be effective,(7) while 11% receive treatments that are not needed or potentially harmful.(7)
Reducing the gap between evidence and practice is associated with reductions in morbidity and mortality(8-10) and reduced healthcare costs.(11) Therefore, in recent years there has been increased attention on barriers to the translation of research and on how to develop evidence-informed implementation in order to improve patient outcomes.(12-14) Evidence is now also needed on effective implementation of primary prevention of NCDs in different contexts through policies and intersectoral health promotion.
Want to conduct your own implementation science project? Download this project proposal template and fill it out as you move through the steps below.
-
Step 1: Identifying evidence-based policies & interventions appropriate to your local context
Before a policy or intervention is selected and implemented it is important to ascertain that there is a need for it and that there is enough high quality evidence to suggest that it will be effective in the local context.
View -
Step 2: Adapting and piloting the policy or intervention
The interplay between a policy or intervention and its local context can impact both its implementation and its effectiveness. This means that a policy or intervention may need some adaptation.
View -
Step 3: Evaluating the implementation of a policy or intervention
Planning and focused efforts to evaluate the implementation of NCD policies and interventions is essential. The evaluation should look at the implementation of policies and interventions as well as their effectiveness.
View -
Step 4: Scaling up a policy or intervention
Once a policy or intervention has been implemented and evaluated successfully, there may be interest scaling-up. ExpandNet and WHO have worked together to develop a nine step guide for developing a scaling-up strategy.
View
Resources and Readings to support Implementation Science
Website resources
These resources provide a variety of support for implementation science. Visit these websites to learn more about implementation science, ongoing projects in the field, funding & networking opportunities, and much more.
- Strengthening capacity for NCD implementation research in the WHO Euro Region
- NIH ODD Dissemination & Implementation ResourcesLibrary of federal tools and resources
- NIH Fogarty Implementation ScienceNews, resources & funding for global health
- NCIDCCPS Implementation Science TeamCancer control training, research tools & funding opportunites
- Cancer Control P.L.A.N.E.T.Design, implement & evaluate evidence-based cancer control programs
- Implementation Science JournalOpen access, peer-reviewed online journal
- Implementation Research PlatformSource of implementation research knowledge and strategies
- Implementation Science ExchangeTools for executing implementation science research projects
- WHO TDR Implementation ToolkitConducting implementation research projects for diseases of poverty
- Research-Tested Intervention ProgramsSearchable database of evidence-based cancer control interventions/programs
- ExpandNetSupport for the science & practice of scale-up
- US VA Health Services Research & DevelopmentImplementation science publications, reports & cyberseminars
- Active Implementation HubOnline learning environment for implementation & scale-up of programs
- Australia Cancer Implementation Science Community of Practice
- Training Institute for Dissemination and Implementation Research in Cancer (TIDIRC)Online training modules and materials
- Implementation Research InstituteCareer development resources for implementation science in mental health
- University of Washington Implementation Science Resource HubGet connected with others in the field and explore research resources
Stakeholder Engagement & Community Participation
These resources provide practical guidance for engaging stakeholders and the community.
Grantsmanship Websites
If you are looking to apply for a grant for your own implementation research project, check out these resources for guidance and examples.
Textbooks
- Brownson RC, Colditz GA, Proctor EK. (2018). Dissemination and Implementation Research in Health: Translating Science to Practice (2nd ed). New York: Oxford University Press, Inc.
- Straus S, Tetroe J, Graham I. (2013). Knowledge Translation in Health Care: Moving from Evidence to Practice. Wiley-Blackwell.
- Grol, R., Wensing, M., Eccles, M., & Davis, D. (Eds.). (2013). Improving patient care: the implementation of change in health care. John Wiley & Sons.
Overview of Implementation Science
- Bauer M. et al. (2015). An introduction to implementation science for the non-specialist. BMC Psychology. 16(3):32.
- Glasgow R, et al. (2012). National Institutes of Health Approaches to Dissemination and Implementation Science: Current and Future Directions. American Journal of Public Health, 102(7): 1274-1281.
- A guide to implementation research in the prevention and control of noncommunicable diseases Chapter 2
Identifying the Implementation Problem, Aims & Questions
- A guide to implementation research in the prevention and control of noncommunicable diseases Chapter 3.1
Models, Theories and Frameworks: Design and Implementation
- Nilsen P. (2015). Making sense of implementation theories, models and frameworks. Implementation Science, 10:53.
- Tabak R. et al. (2013). Models in dissemination and implementation research: useful tools in public health services and systems research. Frontiers in Public Health Services and Systems Research, 2:1.
- Feldstein, A. C., & Glasgow, R. E. (2008). A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. The Joint Commission Journal on Quality and Patient Safety, 34(4), 228-243.
- Damschroder L, et al. (2009). Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science, 4:50.
- Aarons G, et al. (2014). Mixed-methods study of a conceptual model of evidence-based intervention sustainment across multiple public-sector service settings. Implementation Science, 9:183.
- Dissemination & Implementation Models in Health Research & Practice website
- Consolidated Framework for Implementation Research (CFIR) website
- Advanced Topics in Implementation Science Webinar Recordings on D&I Models:
- Consolidated Framework for Implementation Research (CFIR) by Laura Damschroder
- Exploration, Preparation, Implementation, Sustainment (EPIS) by Greg Aarons
- Interactive Systems Framework (ISF) by Abe Wandersman
- Knowledge to Action Framework (KTA) by Sharon Straus
- Promoting Action on Research Implementation in Health Services Framework (PARIHS) by Alison Kitson & Gill Harvey
Models, Theories and Frameworks: Evaluation
- Glasgow R. et al. (1999). Evaluating the Public Health Impact of Health Promotion Interventions: The RE-AIM Framework. American Journal of Public Health, 89:9.
- Normalization Process Theory
Study Design
- Brown, CH, et al. (2017). An overview of research and evaluation designs for dissemination and implementation. Annual Review of Public Health, 38:1-22.
- Creswell JW, Klassen AC, Plano Clark VL, and Smith KC for the Office of Behavioral and Social Sciences Research. Best practices for mixed methods research in the health sciences. (2011). National Institutes of Health.
- Curran G, et al. (2012). Effectiveness- implementation Hybrid Designs: Combining Elements of Clinical Effectives and Implementation Research to Enhance Public Health Impact. Medical Care, 50(3): 217-226.
- Palinkas L, et al. (2011). Mixed Method Designs in Implementation Research. Administration and Policy in Mental Health, 38:44-53.
Study Measures
- Lewis A, Procotr EK, Brownson R. (2018). Measurement Issues in Dissemination and Implementation Research (Chapter 14). Brownson R. et al. Dissemination and Implementation Research in Health: Translating Science to Practice. New York: Oxford University Press.
- Rabin B, et al. (2016). Measurement resources for dissemination and implementation research in health. Implementation Science, 11:42.
- Proctor E, et al. (2011). Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Administration and Policy in Mental Health, 38:65-76.
- Chaudoir SR, and Dugan AG. (2011). Dissemination and implementation measurement compendium: A systematic review of structural, organizational, provider, patient, and innovation level measures. Report submitted to Connecticut Institute for Clinical and Translational Science; Center for Health, Intervention, and Prevention; University of Connecticut.
- Martinez R, Lewis C, Weiner B. (2014). Instrumentation issues in implementation science. Implementation Science, 9:118
Grant Writing/Funding
- Proctor, EK. et al. (2012). Writing implementation research grant proposals: 10 key ingredients. Implementation Science. 7:96.
- Brownson et al. (2015). Concocting that Magic Elixir: Successful Grant Application Writing in Dissemination and Implementation Research. Clinical and Translational Science, 8(6):710-716.
Cultural Adaptation & Fidelity
- Gonzales Castro F, Yasui M. (2017). Advances in EBI Development for Diverse Populations: Towards a Science of Intervention Adaption. Prevention Science, 18:623-629.
- Allen J, Shelton R, Emmons K, Linnan L. (2018). Fidelity and Its Relationship to Implementation Effectiveness, Adaptation, and Dissemination (Chapter 16). Dissemination and Implementation Research in Health: Translating Science to Practice. New York; Oxford University Press.
- Baumann A, Cabassa L, Wiltsey-Stirman S. (2018) Adaptation in Dissemination and Implementations Science (Chapter 17). Brownson R et al. Dissemination and Implementation Research in Health: Translating Science to Practice. New York; Oxford University Press.
- A guide to implementation research in the prevention and control of noncommunicable diseases Chapter 3.2
- Rabin BA, McCreight M, Battaglia C, et al. (2018). Systematic, Multimethod Assessment of Adaptations Across Four Diverse Health Systems Interventions. Frontiers in Public Health, 6:102.
- Stirman SW, Miller CJ, Toder K, Calloway C. (2013). Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implementation Science, 2013(8). 10.1186/1748-5908-8-65
- Gonzales N. (2017). Expanding the Cultural Adaptation Framework for Population-Level Impact. Prevention Science, 18(6) 689-693.
Implementation Strategies
- Kirchner J, Waltz T, Powell BJ, Smith JL, Proctor EK. (2018). Implementation Strategies (Chapter 15). Brownson R et al. Dissemination and Implementation Research in Health: Translating Science to Practice. New York; Oxford University Press.
- Powell BJ, et al. (2015). A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implementation Science, 12:10.
- Proctor EK, Powell BJ, McMillen JC. (2013). Implementation strategies: recommendations for specifying and reporting.Implementation Science, 8:139.
- Powell BJ, et al. (2017). Methods to Improve the Selection and Tailoring of Implementation Strategies. Journal of Behavioral Health Services, 44(2):177-194.
Information on and resources from past and future capacity-building opportunities
Upcoming Training Opportunities
GACD Implementation Science School: Bangkok, Thailand – 5-9th November 2019
GACD 2019 Implementation Science School Webinar
GACD 2019 Webinar Slides
GACD Training School Readings and Resources
Day1 Break-out session slide template
GACD Implementation Science Workshop: Bangkok, Thailand – 11-12th November 2019

Past Training Programs
GACD Implementation Science School:
Campinas, Brazil – 6-10 November 2018
2018 Implementation Science School Programme
GACD Implementation Science Workshop:
Sao Paulo – 12-13 November 2018
ImpSci Day1
ImpSci Day2
GACD Implementation Science Workshop:
Tokyo – 5-7 July 2018
Tokyo Workshop Agenda
Overview of Implementation Science
Selecting appropriate study design & measurement for your project
Case examples of IR 1
Case examples of IR 2
Roundtable Questions
Roundtable Prof Katsunori Kondo
Roundtable Dr Yoko Izumi
Other Training Materials
Implementation Science Overview Lecture
Training Institute for Dissemination and Implementation Research in Cancer (TIDIRC)
These real-world case studies provide examples for how implementation science can be conducted to combat diverse global health problems in a variety of settings
-
Case Study 1
Carrying out a situational analysis for the implementation of NCD prevention and control policies and interventions
-
Case Study 2
Knowledge synthesis on plain packaging to assess existing evidence to promote the selection of evidence-based policies and interventions for implementation in India
-
Case Study 3
Adapting policies and interventions to new contexts – Hypertension, Mongolia
-
Case Study 4
The importance of establishing acceptability – Respiratory diseases, Senegal
-
Case Study 5
Why do we need to assess reach as well as effectiveness? – Diabetic foot, India
-
Case Study 6
Scaling up of physical activity interventions at the national level in Brazil: An effective solution to increase physical activity at the population level

