Excess cost of care associated with sepsis in cancer patients: Results from a population-based case-control matched cohort
A new research article led by Dr Michelle Tew quantifying the excess cost of care associated with sepsis in cancer patients was published in PLOS One. This research was conducted in collaboration with Professor Kim Dalziel and Professor Philip Clarke from the Health Economics Unit, Professor Karin Thursky from Peter MacCallum Cancer Centre and collaborators from Toronto (Professors Murray Krahn, Lusine Abrahamyan and Andrew Morris).
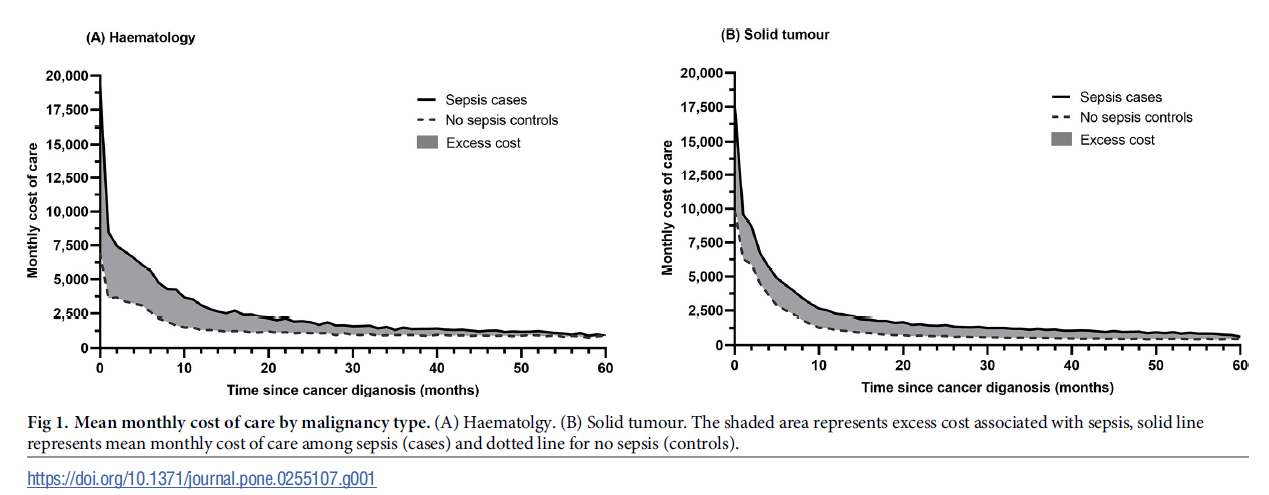
The study used patient-level administrative data from more than 75,000 cancer patients in Ontario, Canada to estimate the whole of system healthcare cost of cancer patients with and without sepsis. A key takeaway is that sepsis is common in patients with cancer, and it is a high cost, high mortality condition imposing substantial burden on the healthcare system as well as on the patients. The cost of care of cancer patients who developed sepsis is substantial–up to 90% higher compared to patients without sepsis. This translated into an excess cost associated with sepsis of CAN$29,081 in the first year, rising to CAN $60,714 over 5 years for solid malignancies. This was higher for haematology; CAN $46,154 in the first year, increasing to CAN $75,931 after 5 years. The highest cost was incurred in the first year of cancer diagnosis which reflects the intensive treatments required, and also reflects the period where patients are at increased risk of developing sepsis. Therefore, there is a need to strengthen initiatives for prompt sepsis identification and treatment particularly in the first year of cancer diagnosis, and in managing and preventing subsequent sepsis episodes. These cost estimates are helpful in informing resource allocation and health policy prioritisation considerations and can also be used in cost-effectiveness models for decisions on sepsis interventions. They are useful in helping inform development of sepsis programs and policies across the cancer care continuum, which can include prevention, screening, treatment and end-of-life care.
Click to enlarge diagram