This report outlines results from our survey of disability support workers (DSWs) and their experiences during the COVID-19 pandemic, conducted in May-June 2020. This is the on-line version of the research findings. You can also download additional reports about the Disability Support Workforce and COVID-19 in the menu on the left.
Summary
DISABILITY SUPPORT WORKERS: THE FORGOTTEN WORKFORCE IN COVID-19 describes the findings from a national survey of 350 disability support workers (DSWs) conducted between May and June 2020.
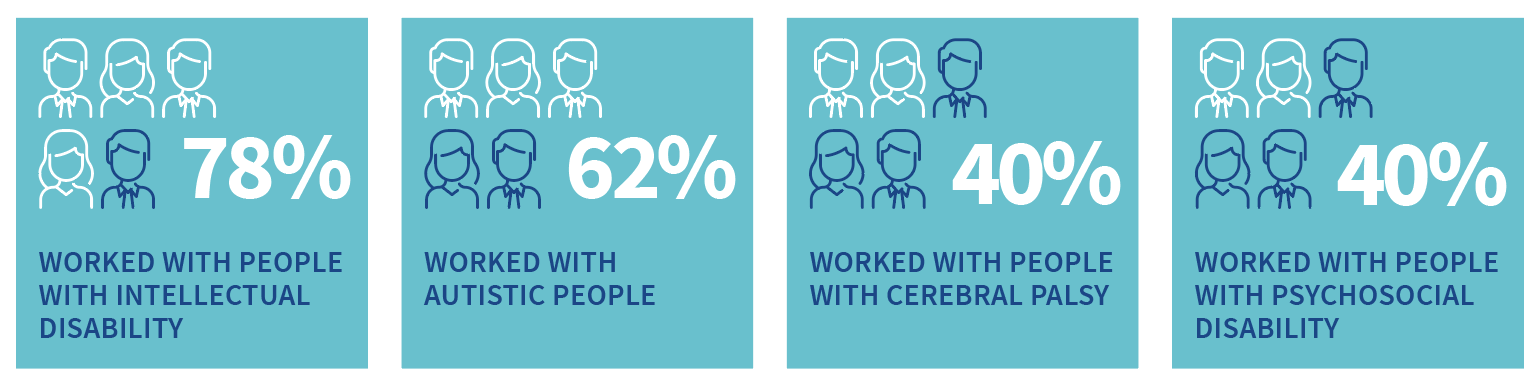
Disability Support Workers were asked about work-related issues such as; how they managed physical distancing, COVID-19 infection control training, access to Personal Protective Equipment (PPE), testing, who they worked with and where they provided support and, the financial and psychological impacts of working during COVID-19.
Like health and aged-care workers, support workers can’t physically distance given the close personal contact required in their job, and because they work with an average of six people with disability a week. The survey also found that support workers faced significant financial hardship. Of those who took time off due to illness, only 47% were paid, reflecting the workforce’s casual nature. 34% were not able to pay an electricity, gas or phone bill on time or being unable to pay their rent.
The survey also found that:
- 53% provided support with tasks that require close personal contact like feeding and brushing teeth
- 23% had not received any COVID-19 infection control training
- Of the 77% who did receive training, 48% would like more
- 64% had received or purchased some form of personal protection equipment (PPE). More than half (54%) received gloves and 37& masks from their employer. Notably, 38% purchased their own masks
- 23% had been tested for COVID-19 infection and 11% wanted to be tested
- 14% worked for more than one provider and six per cent worked in both the aged-care and disability sector
- 30% worked in two or more settings, and 14% worked in three or more settings
- 27% cancelled shifts because they were worried about COVID-19 infection and 35% had shifts cancelled by clients or employers due to fear of COVID-19
- 16% reported high psychological distress levels consistent with serious probable mental illness; 22% of workers experiencing financial stress had probable mental illness, compared to 14% among those who did not report financial problems.
The results reflect the situation for workers when PPE was just being made available to workers after a marked shortage in March and April. With cases now rising in Victoria, on 17 July PPE became compulsory for DSWs in hot spot areas. The researchers have made recommendations, including updating PPE guidelines, proactively reaching out to DSWs so they can receive the required training, ensuring they have access to pandemic leave and making sure expert health staff can provide back-up if needed.
The Research Report contains important findings for governments, services, people with disability and their support workers on preventing COVID-19 transmission in the disability community.
Lead researcher Professor Anne Kavanagh who is Chair in Disability and Health and Academic Director of the University’s Melbourne Disability Institute, said the situation in Victoria was serious with increasing numbers of COVID-19 in disability group homes and among support workers.
COVID-19 really emphasised in my mind how overlooked the disability sector is. At the beginning the government kept talking about health care workers and nursing homes but I never heard any mention of disability. It left us in unknown territory and felt like we had just been forgotten and weren’t as important as other workers
(Survey participant).
Survey Results
Who participated?
357 DSWs from around Australia; 83% were women and 81% were born in Australia. DSWs ranged in age from 18 to 75 years, with 31% over the age of 50 and 7% over 60 years of age. It is worth noting that, older workers are at more risk of complications if infected with COVID-19
Physical distancing
- 90% of disability support workers said they were NOT able to physically distance at work
- 53% provided support with tasks that require close personal contact like feeding and brushing teeth
Like health and aged-care workers, DSWs are unable to physically distance because of their work. This means that they need to wear masks at all times and possibly N95/P2 masks if there are concerns regarding assisting with tasks that generate aerosols.
COVID-19 infection control training
- 23% of workers had NOT received any COVID-19 infection control training and 69% of those wanted more training
- Of the 77% of workers who did receive training, 48% would like more training
- Most workers who received training had online training (66%) and/or printed material (26%)
Use of Personal Protective Equipment
- 64% of DSWs had received or purchased some form of PPE.
- Over half (54%) had received gloves and 37% received masks (surgical and/or N95/P2) from their employer. Notably, 38% of DSWs purchased their own masks even if they had some from their employer.
The chart below (Figure 1) shows the proportion of DSWs who received PPE from their employer and proportion who purchased PPE themselves by type of PPE.
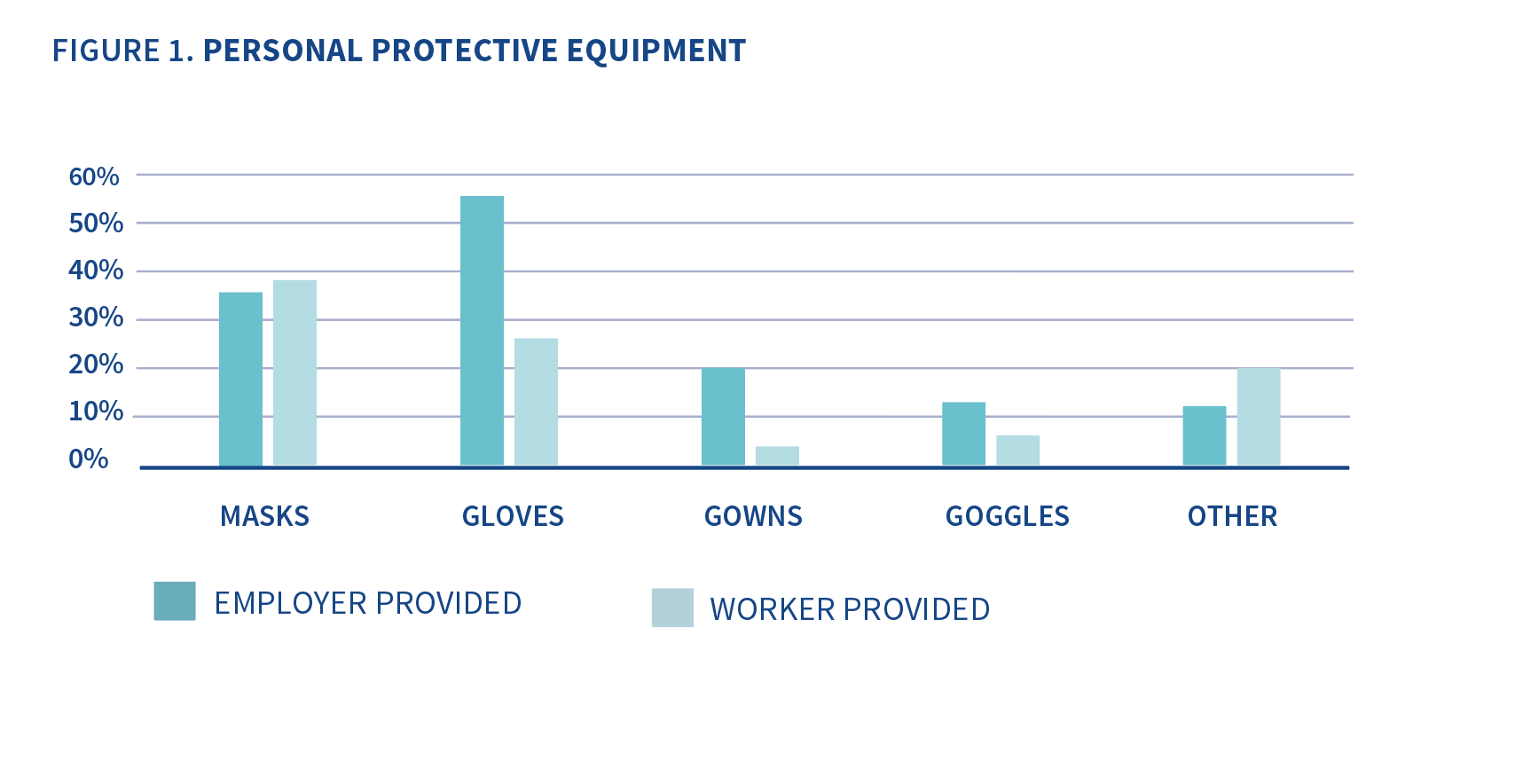 Of the DSWs who had acquired PPE, 59% had received some PPE from their employer for free and 90% had purchased some PPE themselves. 59% workers received PPE from their employer and also purchased PPE themselves. 4% reported that they didn’t receive any PPE from their employer. 41% didn’t purchase any PPE for themselves.
Of the DSWs who had acquired PPE, 59% had received some PPE from their employer for free and 90% had purchased some PPE themselves. 59% workers received PPE from their employer and also purchased PPE themselves. 4% reported that they didn’t receive any PPE from their employer. 41% didn’t purchase any PPE for themselves.
COVID-19 symptoms and testing
23% of workers had been tested for COVID-19 infection and 11% had wanted to be tested citing a range of reasons including ‘they did not have symptoms’, ‘they did not meet the criteria for testing’ even though they may have had symptoms, or they didn’t want to take time off work to wait for the results.
When time was taken off work because a worker was sick only 47% were paid, reflecting the highly casualised nature of this workforce.
Financial impacts on Disability Support Workers
Where they worked
- 14% of DSWs reported that they worked for more than one provider.
- 6% of DSWs worked in both the aged-care and disability sector.
- DSWs worked with an average of 6 people with disability in the week previous to the survey with a range of 0 to 50 people.
DSWs worked across a number of different settings including private homes, group homes, day programs and supported employment. In the previous week, nearly 60% of DSWs had worked in a group home and nearly half had worked in private homes. A smaller proportion had worked in centre-based activities such as day programs or supported employment.
- 57% of workers provided support in a congregate setting including a group home, centre-based activity or supported employment.
- 30% of workers worked in two or more settings.
- 14% of workers worked in three or more settings.
Financial hardship
- DSWs have been adversely affected financially because of COVID-19.
- 16% of DSWs received JobKeeper and 10% received JobSeeker.
27% cancelled shifts because they were worried about COVID-19 infection and 35% had shifts cancelled by clients or employers because of fear of COVID-19. - 37% worked fewer hours in April than in February 2020 because of COVID-19, 39% worked about the same hours, and 24% worked more hours.
Figure 2 (the chart below) shows the proportion of support workers who experienced different types of financial hardship in April 2020 with the overall levels of reported difficulties in teal and financial difficulties reported by DSWs who experienced a reduction in hours in aqua.
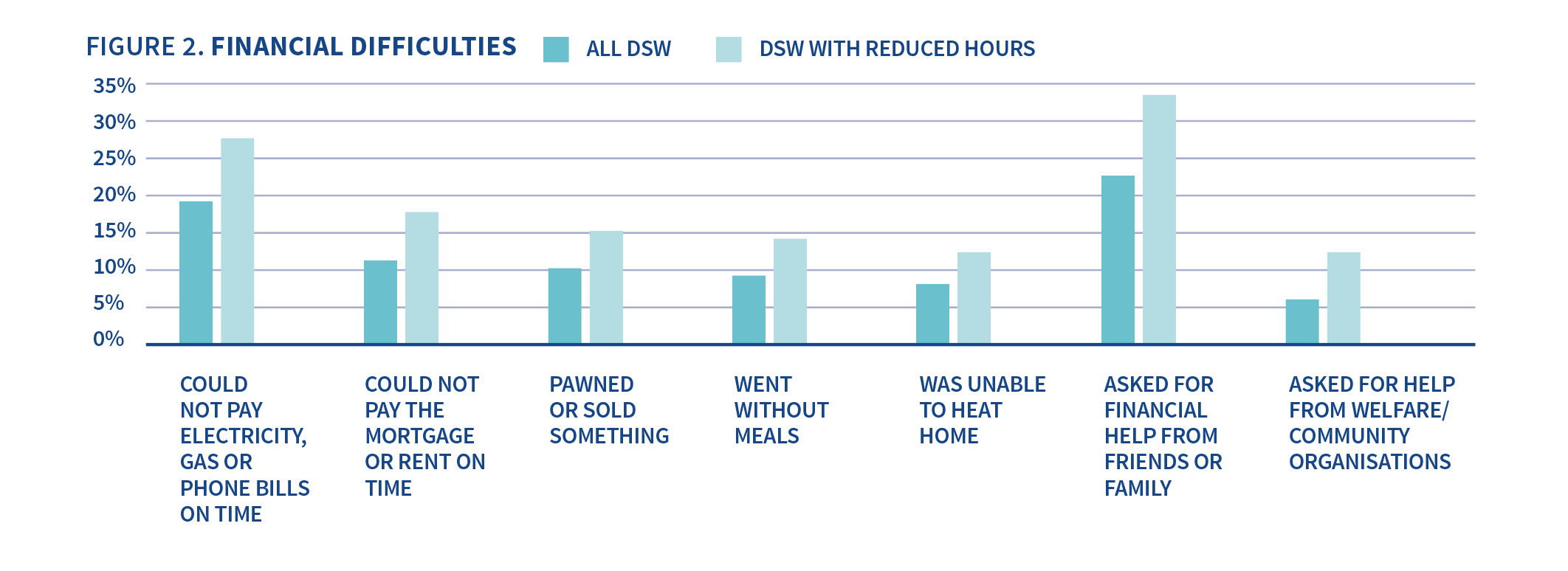
High levels of financial difficulties were reported overall with 17% of workers reporting that they could not pay an electricity, gas or phone bill on time and 20% asking for financial help from family or friends.
Overall, 20% reported that they could not pay a bill, or their mortgage or rent, or went without meals.
Financial difficulties were more frequent among those who reported reduced hours in April with 25% of these workers reporting that they could not pay an electricity, gas or phone bill on time, 16% unable to pay their mortgage or rent, and 13% going without meals. 20% asked for financial help from family or friends. 32% of DSWs who had experienced reduced hours reported that they could either not pay a bill, or mortgage or rent, or went without meals.
Psychological distress and Disability Support Workers
- DSWs are reporting high levels of psychological distress consistent with a clinical diagnosis of anxiety or depression. 16% were shown to have a probable serious mental illness.
- 22% of all workers experiencing financial stress had probable mental illness, compared to 14% who did not report financial hardship.
Concluding Remarks
The results of this survey show the many challenges that the disability support workforce has faced thus far in the pandemic. In places where community transmission is high (currently metropolitan Melbourne and Mitchell Shire in Victoria), the challenges will escalate further. We have made a number of recommendations to support this workforce in the pandemic including proactive reach out for training, access to PPE when required, financial support including paid pandemic leave, priority accessing to testing and mental health support.
These survey results reflect the situation for workers in late May and June when PPE was just being made available to workers after a marked shortage in March and April. Until recently PPE has not been recommended for DSW except when looking after a client who is close contact of a case and is quarantining, has symptoms or is a known case. The situation has changed dramatically since May/June in the context of the rising case numbers in Victoria. On the 17th of July the Commonwealth government stipulated the mandatory use of masks for DSWs in the Victorian hot spot areas, although this is not yet reflected in the national guidelines.
I hope that the disability sector can see the “silver lining” in COVID-19 and see it as an opportunity for increasing the level of professionalism” (DSW survey participant)
There are now also cases of COVID-19 infection among people with disability in group homes. More infections among support workers are also being reported. This presents very real difficulties for workers with little or no training who now have to implement meticulous infection control procedures and use full PPE. Some people with disability, particularly those with psychosocial, autism and/or intellectual disabilities, may find it very challenging to self-isolate or quarantine and may have difficulties with personal hygiene and physical distancing. Further, workers are themselves having to self-isolate or quarantine because they are infected or are a close contact of a case. This means that familiar workers are no longer available to support infected clients at a very stressful time.
Our follow up survey in August 2020 found out more about some of these challenges (See Wave 2 findings report) but in the interim we made a number of recommendations to support the workforce at this time.
Recommendations
- That governments consider updating their guidelines regarding PPE use among DSWs, particularly in areas where community transmission is high.
- That governments are more proactive in reaching out to DSWs so that they receive the training they require. Resources on government websites needs to be more actively promoted. Disability Support Workers need clear information and detailed training about when and how PPE is used, including simulated training not just information online before being expected to work in high risk situations, such as a COVID-positive environment.
- In areas where community transmission is high all support workers should have access to appropriate PPE (minimum of masks) without cost to them. Governments need to make urgent decisions about access to PPE for workers elsewhere in Australia.
- That governments make clear that disability support workers are a priority group for testing along with healthcare and aged-care workers.
- Paid pandemic leave is available to all DSWs who do not have access to paid sick leave and need to self-isolate or quarantine while waiting for a test result; or because they have COVID-19; or are a contact of a known case.
- Governments and providers should ensure DSWs minimise the total number of people they support and the number of settings they provide support in, to reduce risk of transmission among multiple people with disability and support workers, as has been witnessed in aged-care facilities. Particular attention should be paid to identifying workers who work for more than one provider and/or work across multiple group settings.
- Government needs to prioritise ensuring financial security of this essential workforce through extension of JobKeeper or similar supports and paid pandemic leave. Without this, it may not be financially viable for many support workers to remain in their current jobs resulting in an impediment to creating surge capacity in the workforce and an impediment to long term growth.
- Governments and service providers need to provide mental health support to support workers and comprehensive infection control training and access to PPE.
- That governments identify, and have on standby, a skilled health care workforce that can be rapidly deployed to work alongside support workers, or replace them supporting clients infected with COVID-19, as has been deployed in aged-care.
- A surge workforce of support workers fully trained in infection control is created to provide back-up where needed (potentially from later year medical and nursing students).
- That governments and service providers consider options to temporarily rehouse residents in group homes where infections have occurred to separate infected and non-infected residents.
Reports
-
Disability Support Workers: The Forgotten Workforce in COVID-19
Disability Support Workers: The Forgotten Workforce in COVID-19
-
Disability Support Workers: The Forgotten Workforce in COVID-19 (Fact Sheets)
Keeping Disability Support Workers and People with Disability Safe

Financial and Psychological Impacts of COVID-19 on Disability Support Workers

- Disability Support Workers: The Forgotten Workforce in COVID-19 - Wave 2 Findings
- Managing outbreaks in disability residential settings: Lessons from Victoria's second wave
- Vaccine hesitancy among Disability Support Workers
Media
- The Conversation
- ABC News
- SBS news
Acknowledgements
This research was funded by the Melbourne Disability Institute’s COVID-19 funding round at the University of Melbourne. We thank the Advisory Group of Disability Support Workers (DSWs) and the DSWs who participated in the survey for generously giving their time and sharing their insights.
Kavanagh A, Dimov S, Shields M, McAllister A, Dickinson H & Kavenagh M (2020). Disability Support Workers: The Forgotten Workforce in COVID-19 - Research Report. Melbourne: The University of Melbourne. https://doi.org/10.26188/12756428
There are additional reports, including a follow up study to this original research, on the impacts of the pandemic on Disability Support Workers that can be downloaded from this page (see panel on left hand side).