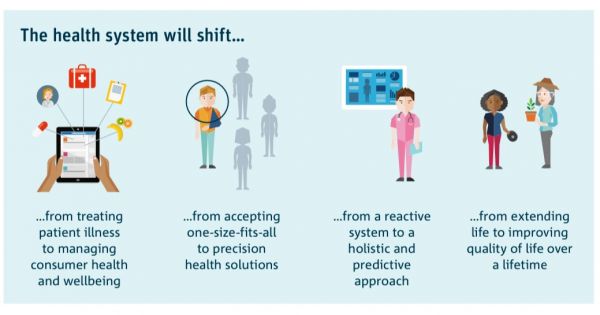
Moving from reactive to predictive: The Future of Health
The CSIRO Future of Health outlines that the health systems in Australia will shift from treating patient illness in the short term to extending life and improving quality of life over a lifetime. The challenge is, how?
Access to health systems can be difficult for patients, and access to managing their healthcare needs is often fragmented. OECD and Menzies Institute reports, focused on Australia, highlight the specific challenges using the term “navigation”. In England, Caught in the Maze by Macmillan Cancer Support similarly highlights the challenges patients experience in accessing and managing their cancer care.
The problems are not new. In the late 1970s Harold Freeman’s work in New York, USA, showed the marked health disparities in breast cancer outcomes between women from different socioeconomic classes. Freeman introduced the term patient navigation, “an intervention to enable access to timely diagnosis and treatment to improve outcomes through removing or reducing barriers to care”.
As a healthcare professional who worked in HIV/AIDS in the 1990s, I was an active part of developing shared care approaches. This approach uses the skills, knowledge and experience of the patient, carer and the health professionals who share joint decision making for an individual's care. But these learnings have never been scaled at a systems level. It was this background and a personal experience of a friend with pancreatic cancer that motivated my Master of Public Health Capstone research to understand the current situation in Australia. If this is a known problem impacting patients every single day, what is being done to address it?
My research highlighted that stakeholders have different areas of focus and the mechanisms for seamless transition are not embedded across the health system. This research has been accepted for presentation at the Canadian Healthcare Navigation Meeting in April.
My PhD research, in Australia and England, will build on the above and aims to identify the mechanisms and incentives that are being developed and deployed to enable patients to access and manage their healthcare across the levels of health and how these mechanisms are incentives are being measured.
Siân Slade is a PHD student at the Nossal Institute. She is a UK-trained pharmacist, MPH, MBA, GAICD qualified and a PhD researcher in global health systems. Siân is being supervised by Professors Barbara McPake, Peter Brooks, Adam Elshaug at the University of Melbourne and Mr James Sanderson, NHS England and Improvement.