Remote Area Eye Care: A Personal Story.
This 'Share Your Story' was written by Kerry Woods, Aboriginal Eye Health Coordinator at Lions Outback Vision.
BACKGROUND
Lions Outback Vision travels the State of Western Australia from Albany through to Wyndham stopping in rural and remote towns to address the effects of vision loss and blindness. Outreach services are coordinated visits by ophthalmologists to regional communities primarily in locations which host a regional hospital or medical centre where surgical procedures can be performed. Lions Outback Vision works closely with WA Country Health Services, Population Health Networks, Aboriginal Medical Services, local health organisations and community groups.
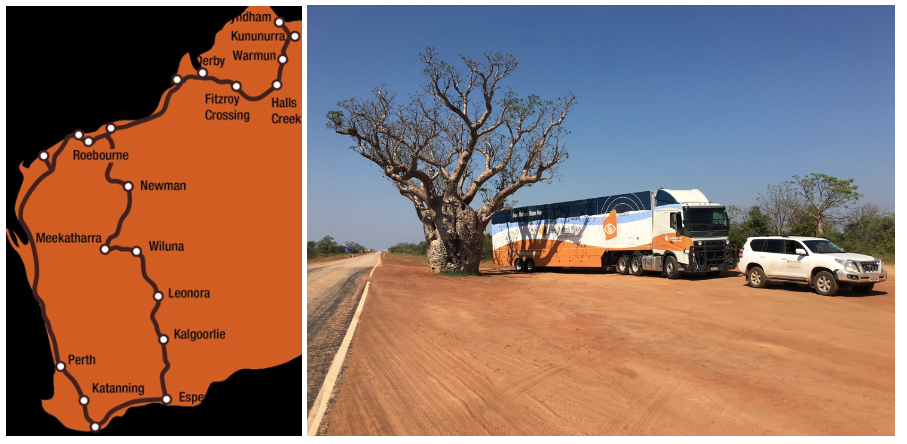
Image: Outreach service locations
My name is Kerry Woods (Everett) and I am an Aboriginal woman from the clan Plangermairreenner of the Ben Lomond people a clan of the Cape Portland nation in North-East Tasmania. I have been living in Noongar country (Perth) for the past 20 years and I currently work with the Lions Outback Vision team.
My role as the Aboriginal Eye Health Coordinator is to help assist Aboriginal patients across the state to attend ophthalmology appointments on the vision van and if needed, coordinate the patients coming from country to Perth for eye surgery.

Image: Kerry on the road
During the Kimberley Vision Van circuit an Aboriginal patient from a remote community attended for an eye appointment. The community is located 2 ½ hours away and requires transport to be organised well in advance for patients to attend. This is a small bus which, if it is full, means the patient can miss out on their appointments. This patient previously had cataract surgery 6 weeks prior to this appointment. The day 2 post-operative review identified an intraocular pressure (IOP) rise which settled, followed by another review by a visiting optometrist with the IOP dropping even further but still within the accepted range. The patient attended his appointment on the Vision Van with his partner. I was the first person to greet the patient after which he started to explain to me, he was suffering severe pain in his eye that had recently been operated on, so much so that he was holding his hand over his eye and struggled to open it.
I immediately proceeded to check his vision and eye pressure. The IOP registered at 53, well above the range expected. The patient was struggling with the pain, and I felt it was important to interrupt the doctor to inform him of the abnormally high readings. The doctor re-checked the patients IOP readings, and the result was the same. The patient was provided with a script for oral medication to reduce his IOP which was to be reviewed in 2 days. This was made possible by the Vision Van being in town for the week, which allowed the patient to be monitored and follow up care provided in an appropriate timeframe. Without this service available in town at the time, the patient would have been flown to Perth.
The patient was seen 4 days later, informing us he had been unable to take the medication due to nausea. His IOP level was at 35 and he was still in severe pain. Alternative treatment was explained to the patient, to which he agreed. I was asked to accompany the patient in preparation for the treatment, so I could counsel the patient and comfort him. I assisted the doctor during the procedure to help keep the patient still by holding his hands at first, and then continually talking to him for reassurance and calmness. This was a difficult situation as the treatment being provided was necessary but also painful even with the anaesthetic. Once the treatment was provided the pain subsided for a short while and then rose again, making it difficult for the patient to manage which made him quite vocal. The ophthalmologist requested I take the patient to the emergency department to have his pain treated while he organised for the patient to be transferred to Perth for surgery. I rushed the patient and his partner to the hospital and had him admitted within moments of arriving and after a short time he was given pain relief. Once the patient’s pain subsided, I was able to explain in detail the procedure he had received on the Vision Van and what he had experienced from that treatment. I discussed the next steps for his transfer to Perth for surgery and let him know I was available to talk to them anytime. After the patient felt comfortable, I organised food and then assisted his partner in accessing accommodation through the Patient Assisted Travel Scheme (PATS). I made sure the PATS paperwork was completed and informed PATS that the patient would be transferred to Perth, and he would need his partner to attend.
The patient and his partner travelled to Perth, and he underwent an urgent Molteno tube surgery a drainage device to reduce his IOP levels. I kept in contact with the patient during his stay in Perth and once he returned home. The first few weeks post-surgery he was still experiencing pain and so I liaised with the ophthalmologist to make sure his eye was healing as expected. Due to the patient’s experience with severe pain and emergency surgery he relied on me to be available when he had questions or was unsure about something. This included after hours and weekends. Once he returned home, he continued with the calls to discuss upcoming appointments, medication and his general wellbeing. I reschedule his appointments with us if it clashes with his community obligations and I make sure transport is available. The patient has slowly recovered and is following his treatment plan.
After the Vision Van left town, the patient still needed to have regular eye checks to make sure the drainage tube was working. I contacted an optometrist in Broome and scheduled an appointment for the patient to have a quick IOP check done. I was informed that this would cost the patient as it wasn’t covered by Medicare. Fortunately, I was able to discuss the patient’s situation and he was offered an appointment with no cost.
During the time spent with the patient and his partner I was able to build a trusting relationship where we discussed family, country and connections through people we know. The patient had previously visited my country and remarked how beautiful it is, he had met some of my countrymen and wanted to return to Tasmania to reconnect with them
From the first meeting on the Vision Van this patient and his partner recognised me as another Aboriginal person and immediately had a connection. His partner would whisper sensitive information to me while waiting to be seen. They gave me honest answers regarding their past lifestyles knowing that I wasn’t about to judge them. I felt privileged as he was entrusting me with facts about his life, and with consent I was able to pass on information to the doctor for the benefit of his medical treatment. In this situation this patient felt culturally safe and secure which ultimately led to the success of his health outcome. During one of our many conversations he invited me to visit One Arm Point to meet with the community and talk about eye health. He feels he has learnt a lot from his experiences and wants that information passed onto the community.

Image: Kerry embracing a patient
This was a unique case where a patient had an acute pressure rise in his eye secondary to diabetic eye disease, which had been difficult to manage despite the oral medication. It was a traumatic experience for the patient, his partner and for me seeing and hearing a person in extreme pain and not being able to immediately relieve it. I feel that in this unusual situation, I was able to build up trust with the patient and his partner and felt that my knowledge and experience with eyes helped the patient to understand his eye condition and the importance of the treatment.
If you have any questions relating to this ‘story’ please contact Kerry Woods, Aboriginal Eye Health Coordinator at Lions Outback Vision via email KerryWoods@lei.org.au or telephone (08) 9381 0802.
This 'Share your Story' article was published 19 March 2020.